Urinary urgency, discomfort and slowing of the urine stream should never be dismissed as just a part of growing older. Such symptoms usually indicate treatable health conditions and, in some cases, they signal damage to the urethra, the tube that carries urine from the bladder out of the body.
Urinary dysfunction—including urinary urgency, discomfort and slowing of the urine stream—should never be dismissed as a normal progression of aging. Such symptoms may indicate real and treatable health conditions, such as a urinary tract infection or prostate disease or, in some cases, they may signal damage to the urethra, the tube that carries urine from the bladder out of the body. Men experiencing these symptoms are advised to visit their physician or urologist.
If infection or prostate enlargement is ruled out as the cause of the urinary dysfunction, your urologist will test for stricture, or narrowing, of the urethra. The male urethra is nearly eight inches long, making men far more prone to stricture than women, in whom the urethra is only about an inch-and-a-half long.
Though the condition can affect men at any age, it is most frequently found in men over age 65. Urethral stricture may be caused by inflammation or scar tissue resulting from traumatic injury to the pelvic area and from untreated infections, including sexually transmitted disease, yet in many cases the precise cause of the narrowing remains unknown. Left untreated, the condition can lead not only to increased discomfort, but also to an increased risk for infections that could ultimately result in bladder and kidney problems.
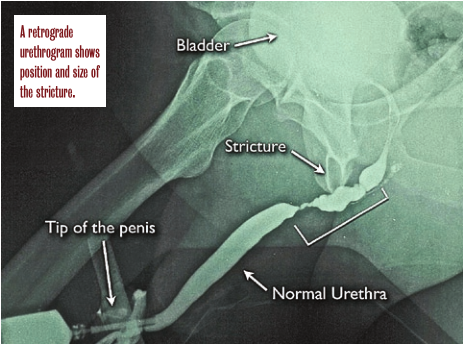
Strictures are typically found on cystoscopy. To confirm a urethral stricture and gauge the location and size of the narrowed area, Premier Medical Group Urologist Walter Parker, M.D. orders a retrograde urethrogram. This simple test involves taking an x-ray of the patient’s urethra and bladder following injection with a contrast dye. Based on the results of the urethrogram, Dr. Parker can determine whether the patient may get relief from standard first options, such as catheter dilation to enlarge the narrowed area and endoscopic urethrotomy. If the stricture is too large or the tissue is permanently damaged, he may recommend reconstructive surgery, known as urethroplasty, to open the blockage.
The Urethroplasty Procedure
The first surgical procedure for repair of a urethral stricture was described in a medical journal in 1914, one hundred years ago. In contemporary times, several surgical options are available. A patient with a simple stricture (generally 1 cm or less in length) may be a candidate for what is called a primary (or anastomotic) urethroplasty. During this procedure, Dr. Parker excises the diseased tissue that is constricted and reconnects the remaining segments of the urethra. The procedure typically requires overnight hospitalization and use of general anesthesia.
Patients with complex strictures may need a more extensive surgery, known as substitution (grafting) urethroplasty, in which Dr. Parker cuts the narrowed portion of the urethra lengthwise and grafts tissue from the lining of the patient’s mouth to the excised area to enlarge it. Dr. Parker points out that this mucosa tissue is easily obtained, does not scar, is resistant to infection and usually heals quickly. In the case of a severe stricture, the grafting may have to occur in stages.
Substitution urethroplasty is, in most cases, performed in an operating room under general or spinal anesthesia. Recovery time is generally four weeks. Risks from the operation include those associated with any surgery, including bleeding and infection. There is also a slight risk of sexual dysfunction following the procedure, although studies indicate urethral reconstruction appears no more likely to cause long-term postoperative sexual dysfunction than does circumcision.
Some patients may have a repeated re-occurrence of the stricture when treated with non- surgical methods, but the odds of this are significantly lower following reconstructive surgery. “Urethroplasty is not a simple procedure and it requires the expertise of a skilled urologist,” Dr. Parker says. “The recovery period is significant. But when successful, as it generally is, the procedure offers patients long-term relief.”