Can a Vasectomy be Reversed?
Yes, vasectomies can be reversed even after very prolonged periods of time, sometimes after more than 20 years. Sperm are constantly being produced in men and even after time, there should be viable sperm. But microsurgical vasectomy reversal can be relatively expensive and there are no guarantees of returned fertility.
What is the Success Rate of a Vasectomy Reversal?
Microsurgery results in return of sperm in 75 to 97% of patients.
How Common are Vasectomy Reversals?
Like many things in life, circumstances change and approximately 6% of patients who undergo vasectomy subsequently desire to father children. Each year about 30,000 men in the United States will have their vasectomy reversed. The reasons for vasectomy reversal vary, but it is safe to say at the time of their vasectomy these men never suspected they would want to have it reversed.
Besides Vasectomy Reversal, are There any Other Options? How do the Costs Compare?
The other option is to extract a small amount of tissue from the testes or epididymis, referred as testicular sperm extraction (TESE) and microsurgical epididymal sperm extraction (MESA) respectively. Sperm may be isolated from this tissue and used in conjunction with In Vitro Fertilization (IVF). But the cost of a vasectomy reversal is significantly less than the cost of IVF and sperm retrieval surgery. In fact, parents will typically spend two to three times as much on IVF than vasectomy reversal for each baby born.
How is Vasectomy Reversal Performed?
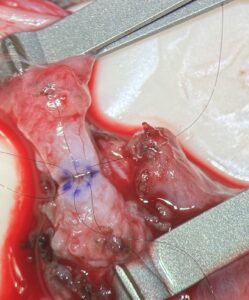
Vasectomy reversal is performed by a surgical technique called microsurgical vasovasostomy . The surgery is performed under general anesthesia and uses an operative microscope that provides substantial magnification to visualize the vas deferens. While the vas deferens itself is small, about the size of a piece of spaghetti, it is the lumen, or channel, inside the vas which is microscopic. The diameter of this inner channel is 500 micrometers, 1/2 the length of a millimeter. The surgeon then reattaches each end of the vas deferens using what is known as a 3-layer anastomosis: the lumen and surrounding muscle layer are reconnected in 2 separate steps using microsurgical 10-0 nylon and 9-0 nylon, followed by a third layer using microsurgical 7-0 nylon. This technique is the gold standard method of reattachment and is generally preferable to a modified 1-layer technique.
What About the Complex Repair?
During a vasectomy reversal, the fluid, where the prior vasectomy site is identified, is tested for the presence of sperm. If no sperm is identified and the fluid is thick and pasty, it signifies a second blockage closer to the testicle, at the level of the epididymis. In these situations, a vasovasostomy would only relieve one of the blockages and, instead, a vasoepididymostomy, a more complex repair, is performed. Bypassing both blockages, the vas deferens is surgically connected to a location on the epididymis above the obstruction. This technique is generally considered more “complex” because there is significant asymmetry between the size of the small vas deferens lumen and size of the miniscule epididymal tubule, resulting in overall lower postoperative patency rates for vasoepididymostomy compared to vasovasostomy.
What is the Recovery and Healing from Vasectomy Reversal?
Patients go home the same day from surgery. Postoperative follow-up includes an evaluation of wound healing at 2 weeks and a semen analysis at 6 weeks. A semen analysis is then obtained every 6 weeks until sperm concentration and motility have stabilized—and every three months thereafter until pregnancy is achieved.
For more information, please call to schedule an appointment with our
Vasectomy Reversal Specialist Dr. Jason Krumholtz #845.437.5000
Dr. Krumholtz’s Skilled Microsurgery Gives Men Another Chance at Fatherhood

